

Organ
of the
GD — Society for Dermopharmacy
 |
Issue 1 (2004) |
GD News
GD press release for the prevention of skin cancer
Every year 100.000 new cases of basalioma, spinalioma and melanoma are reported
There is a continuously increasing number of patients suffering from skin cancer. At present far beyond 100.00 persons contract various forms of skin cancer year after year in Germany. Experts count on an annual growth rate of three to eight percent. Accordingly, skin cancer has become a widespread disease thus representing a rising burden for the health care system, reads a press release of the GD Gesellschaft für Dermopharmazie of 31 March 2004. The society drives at generating a public awareness for the prevention of skin cancer and has established an expert group, the GD Task Force “Light.Hautkrebs.Prävention” (Light.Skin Cancer.Prevention) to this end.
Basically three different skin cancer types are distinguished: Basalioma, spinalioma and the malignant melanoma. Basalioma and spinalioma, which are both determined as “light skin cancer” are worldwide the most widespread skin tumours. They appear for the most part at the so-called “sun terraces” such as nose, ears, bald head, lips or in the eye region and moreover at hands and forearms.
Affected by light skin cancer are mainly sunbathers but also construction workers, farmers, seamen or mountain guides who are frequently exposed to the sun over years or decades not at all or insufficiently protected from the sun. Nevertheless, the light skin cancer types are only perceivable in advanced age as the ultra-violet rays of the sun only trigger tumours with a time delay of ten to thirty years.
Basalioma and spinalioma –
most widespread skin cancer types
 The dermatologist professor Dr. med. Thomas L. Diepgen from the department Sozialmedizin, Berufs- und Umweltdermatologie at the Universitätsklinikums Heidelberg (Social Medicine, Occupational and Environmental Dermatology at the University Clinical Center Heidelberg) is speaker of the GD Task Force „Licht.Hautkrebs.Prävention" (Light.Skin Cancer.Prevention). Furtherance of the prevention of skin cancer belongs among other issues to the objectives of this interdisciplinary expert group. |
Basalioma is the most frequent skin cancer type with 80.000 incidences per year; it looks like a small, grey-white knot. Spinalioma as well (approximately 20.000 incidences per year) is in most cases knot-shaped, however more intensely reddened. Already every other person aged 60 and above is affected by the actinic keratosis, also called “rough light callosity” which is considered to be the preliminary stage of the spinalioma. Malignant spinalioma develop from these sub-corneous knots (“sun callosities”) in up to 15 percent of cases.
In the advanced stage basalioma and spinalioma neither spare cartilage nor bones, which may lead in particular to severe disfigurements in the face. Whereas the basalioma continues to grow locally limited, the spinalioma may seize the lymph nodes and form metastases – every tenth case is lethal. “Presumably the light skin cancer types are far more frequent than reported by official statistics”, explains the dermatologist professor Dr. med. Thomas L. Diepgen from the department Klinische Sozialmedizin, Berufs- und Umweltdermatologie at the Universitätsklinikum Heidelberg (Clinical Social Medicine, Occupational and Environmental Dermatology at the University Clinical Center).
Diepgen is speaker of the GD Task Force “Licht.Hautkrebs.Prävention” (Light.Skin Cancer.Prevention) established by the Gesellschaft für Dermopharmazie last year. Furtherance of the prevention of skin cancer, advancement of the research in this field and initiation of the entry of these skin types into the cancer register belong to the objectives of this interdisciplinary expert group.
UV-radiation – risk factor
for the formation of skin cancer
Even more threatening than the light skin cancer types is the malignant melanoma which commences to form metastases already in a very early stage. The tumour may only be a few millimetres thick when it already becomes manifest in distant organs. In the advanced stage the disease is lethal in most cases. Experts estimate that up to 10.000 persons come down with malignant skin cancer every year in Germany at the time being.
The main cause for this significant increase of all skin cancer types is the intense skin contact with the sunlight, according to experts. “The leisure behaviour and the clothing habits have drastically changed in the past decades“, according to Diepgen. In fact, the time share of vacation is less than ten percent; however the UV-radiation by sunlight is in contrast frequently higher than in every-day life. Professor Diepgen: “Above all, exposure to sunlight in the childhood as well as too intense radiation causing sunburns in the course of the vacation have proven to be of particular risk”.
Further important reasons for the rising incidence of skin cancer are the increased life-span of the population as well as the continuous decrease of the ozone layer and the higher UV-exposure of the skin associated with this process.
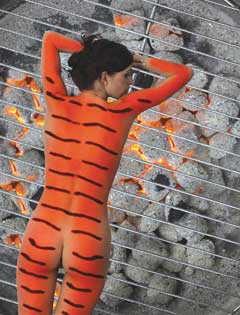 Excessive sunbathing not only entails sunburn but increases at the same time the risk to contract skin cancer. |
Skin cancer as
occupational disease
Occupationally-related skin cancer has been for a long period of time in the focus of medicine. Already 1775, an increased skin cancer risk had been described as one of the first occupational diseases for chimney sweepers. However, it took more than 100 years until 1894 a direct correlation had been drawn for seamen between occupationally-conditioned sun exposure and the formation of skin cancer. Physicians referred to this pathologically modified body surface as ‘seamen skin’.
Nevertheless, skin cancer, caused by intense sun exposure at the place of work is until the present time not considered as occupational disease. However, a process of rethinking seems to take place as professor Diepgen expounds: „In the previous years several skin cancer diseases have been recognized as occupational disease and indemnified. We dermatologists should contribute to a further notification and indemnification of cases and initiate that certain skin diseases induced by UV-light are included in the list of occupational diseases”.
Measures to protect
from skin cancer
Due to the fact that UV-light is particularly concerned in the formation of all skin cancer types, sun protection is the first and utmost protective measure. No matter, whether occupationally or in the private sphere – a protection from skin cancer is feasible. Here are the measures in detail:
top